Esophagheal Cancer

What is esophageal cancer? Cancer that forms in tissues lining the esophagus (the muscular tube through which food passes from the throat to the stomach).Two types of esophageal cancer are squamous cell carcinoma (cancer that begins in flat cells lining the esophagus) and adenocarcinoma (cancer that begins in cells that make and release mucus and other fluids).
Estimated new cases and deaths from esophageal cancer in the United States in 2013:
· New cases: 17,990 reported.
· Deaths: 15,210
- Questions you may want to ask your doctor about surgery
- Do you suggest surgery for me? If so, what type?
- How will I feel after surgery?
- If I have pain, how can we control it?
- How long will I be in the hospital?
- Am I likely to have eating problems? Will I need a special diet?
- Will I need a feeding tube? If so, for how long? How do I take care of it?
- Who can help me if I have a problem?
- Will I have any lasting side effects?
- When can I get back to my normal activities?
More helpful information is available from the following National Cancer Institute
Booklet:
This National Cancer Institute (NCI) booklet is for you – someone who has just been diagnosed with cancer of the esophagus. Another name for this disease is esophageal cancer.
This booklet has lists of questions that you may want to ask your doctor. Many people find it helpful to take a list of questions to a doctor visit. To help remember what your doctor says, you can take notes. You may also want to have a family member or friend go with you when you talk with the doctor—to take notes, ask questions, or just listen.
What is the Esophagus?
The esophagus is a muscular tube in the chest. It’s about 10 inches (25 centimeters) long. This organ is part of the digestive tract. Food moves from the mouth through the esophagus to the stomach.
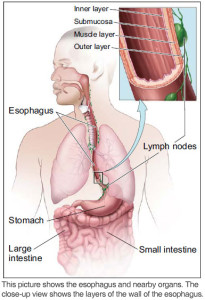
The wall of the esophagus has several layers:
- Inner layer or lining: The lining (mucosa) of the esophagus is wet, which helps food to pass to the stomach.
- Submucosa: Glands in the submucosa layer make mucus, which helps keep the lining of the esophagus wet.
- Muscle layer: The muscles push food down to the stomach.
- Outer layer: The outer layer covers the esophagus.
Cancer Cells
Cancer begins in cells, the building blocks that make up all tissues and organs of the body, including the esophagus.
Normal cells in the esophagus and other parts of the body grow and divide to form new cells as they are needed. When normal cells grow old or get damaged, they die, and new cells take their place.
Sometimes, this process goes wrong. New cells form when the body doesn’t need them, and old or damaged cells don’t die as they should. The buildup of extra cells often forms a mass of tissue called a growth or tumor.
A tumor in the esophagus can be benign (not cancer) or malignant (cancer):
- Benign tumors:
- Are rarely a threat to life
- Don’t invade the tissues around them
- Don’t spread to other parts of the body
- Can be removed and don’t usually grow back
- Malignant tumors (cancer of the esophagus):
- May be a threat to life
- Can invade and damage nearby organs and tissues
- Can spread to other parts of the body
- Sometimes can be removed but may grow back
Esophageal cancer cells can spread by breaking away from an esophageal tumor. They can travel through blood vessels or lymph vessels to reach other parts of the body. After spreading, cancer cells may attach to other tissues and grow to form new tumors that may damage those tissues.
When esophageal cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the original tumor. For example, if esophageal cancer spreads to the liver, the cancer cells in the liver are actually esophageal cancer cells. The disease is metastatic esophageal cancer, not liver cancer. For that reason, it is treated as cancer of the esophagus, not liver cancer.
Types of Esophageal Cancer
In 2013, about 18,000 Americans will be diagnosed with esophageal cancer.
The two most common types are named for how the cancer cells look under a microscope:
- AC: About 12,000 Americans will be diagnosed with AC (adenocarcinoma) of the esophagus in 2013. In the United States, AC is the most common type of esophageal cancer. Usually, AC tumors are found in the lower part of the esophagus, near the stomach. AC of the esophagus may be related to having acid reflux (the backward flow of stomach acid), having a disease of the lower esophagus known as Barrett esophagus, or being obese.
- SCC: About 6,000 Americans will be diagnosed with SCC (squamous cell carcinoma) of the esophagus in 2013. In other parts of the world, SCC is the most common type of esophageal cancer. Usually, SCC tumors are found in the upper part of the esophagus. SCC of the esophagus may be related to being a heavy drinker of alcohol or smoking tobacco.
Tests
After you learn that you have cancer of the esophagus, you may need other tests to help with making decisions about treatment.
Tumor Grade Test
The tumor tissue that was removed during your biopsy procedure can be used in lab tests. The pathologist studies tissue samples under a microscope to learn the grade of the tumor. The grade tells how different the tumor tissue is from normal esophagus tissue.
Tumors with higher grades tend to grow faster than those with lower grades. They are also more likely to spread. Doctors use tumor grade along with other factors to suggest treatment options.
For more about tumor grade, see the NCI fact sheet Tumor Grade.
Staging Tests
Staging tests can show the stage (extent) of esophageal cancer, such as whether cancer cells have spread to other parts of the body.
When cancer of the esophagus spreads, cancer cells are often found in nearby lymph nodes. Esophageal cancer cells can spread from the esophagus to almost any other part of the body, such as the liver, lungs, or bones.
Staging tests may include…
- CT scan: Your doctor may order a CT scan of your chest and abdomen. An x-ray machine linked to a computer will take a series of detailed pictures of these areas. You’ll receive contrast material by mouth and by injection into a blood vessel in your arm or hand. The contrast material makes abnormal areas easier to see. The pictures can show cancer that has spread to the liver, lungs, bones, or other organs.
- PET scan: Your doctor may use a PET scan to find cancer that has spread. You’ll receive an injection of a small amount of radioactive sugar. A machine makes computerized pictures of the sugar being used by cells in the body. Because cancer cells use sugar faster than normal cells, areas with cancer cells look brighter on the pictures. The pictures can show cancer that has spread to the lymph nodes, liver, or other organs.
- EUS: An EUS (endoscopic ultrasound) can show how deeply the cancer has invaded the wall of the esophagus. It can also show whether cancer may have spread to nearby lymph nodes. Your doctor will pass a thin, lighted tube (endoscope) through your mouth to your esophagus. A probe at the end of the tube sends out high-energy sound waves. The waves bounce off tissues in your esophagus and nearby organs, and a computer creates a picture from the echoes. During the exam, the doctor may take tissue samples of lymph nodes.
Stages
Doctors describe the stages of esophageal cancer using the Roman numerals I, II, III, and IV. Stage I is early-stage cancer, and Stage IV is advanced cancer that has spread to other parts of the body, such as the liver.
The stage of cancer of the esophagus depends mainly on…
- How deeply the tumor has invaded the wall of the esophagus
- The tumor’s location (upper, middle, or lower esophagus)
- Whether esophageal cancer cells have spread to lymph nodes or other parts of the body
Stages I and II of Adenocarcinoma of the Esophagus
Stage IA
Cancer has grown through the inner layer and invades the wall of the esophagus. The grade is 1 or 2.
Stage IB
Cancer has invaded the wall of the esophagus and is grade 3. Or, cancer has invaded more deeply into the muscle layer of the esophagus, and the grade is 1 or 2.
Stage IIA
Cancer has invaded the muscle layer of the esophagus, and the grade is 3.
Stage IIB
Cancer has invaded the outer layer of the esophagus. Or, cancer has not invaded the outer layer, but cancer cells are also found in one or two nearby lymph nodes.
Stages I and II of Squamous Cell Cancer of the Esophagus
Stage IA
Cancer has grown through the inner layer and invaded the wall of the esophagus. The grade is 1.
Stage IB
Cancer has invaded the wall of the esophagus and is grade 2 or 3. Or, cancer is found in the lower part of the esophagus, it has invaded the muscle layer or outer layer of the esophagus, and the grade is 1.
Stage IIA
Cancer is found in the upper or middle part of the esophagus, it has invaded the muscle layer or outer layer of the esophagus, and the grade is 1. Or, cancer is found in the lower part of the esophagus, it has invaded the muscle layer or outer layer of the esophagus, and the grade is 2 or 3.
Stage IIB
Cancer is found in the upper or middle part of the esophagus, it has invaded the muscle layer or outer layer of the esophagus, and the grade is 2 or 3. Or, cancer has not invaded the outer layer, and cancer cells are found in one or two nearby lymph nodes.
Stages III and IV of Esophageal Cancer (Both Types)
Stage IIIA
Stage IIIA is one of the following:
- Cancer has not invaded the outer layer, and cancer cells are found in 3 to 6 nearby lymph nodes.
- Or, cancer has invaded the outer layer of the esophagus, and cancer cells are also found in 1 or 2 nearby lymph nodes.
- Or, cancer extends through the esophageal wall and has invaded nearby tissues, such as the diaphragm or pleura. No cancer cells are found in lymph nodes.
Stage IIIB
Cancer has invaded the outer layer of the esophagus, and cancer cells are found in 3 to 6 nearby lymph nodes.
Stage IIIC
Stage IIIC is one of the following:
- Cancer has invaded tissues near the esophagus, and cancer cells are found in up to 6 nearby lymph nodes.
- Or, cancer cells are found in 7 or more nearby lymph nodes.
- Or, the cancer can’t be removed by surgery because the tumor has invaded the trachea or other nearby tissues.
The Treatment
People with cancer of the esophagus have many treatment options. Treatment options include…
You and your doctor will develop a treatment plan. The treatment that’s right for you depends mainly on the type and stage of esophageal cancer. You’ll probably receive more than one type of treatment. For example, radiation therapy and chemotherapy may be given before or after surgery.
At any stage of esophageal cancer, care is available to manage health problems caused by the disease or side effects from its treatment. You can get information about coping with symptoms and side effects on NCI’s website at http://www.cancer.gov/cancertopics/coping.
Also, you can get information about coping from NCI’s Cancer Information Service at 1-800-4-CANCER (1-800-422-6237). Or, chat using NCI’s instant messaging service, LiveHelp (https://livehelp.cancer.gov).
Doctors Who Treat Esophageal Cancer
Your health care team may include the following specialists:
- Gastroenterologist: A gastroenterologist is a doctor like Seema A. Dar, M.D., FACG who is board certified – who specializes in treating problems of the esophagus and other digestive organs.
- Chest surgeon: A chest surgeon (thoracic surgeon) specializes in surgery on the esophagus and other organs inside the chest. You may wish to find an expert in esophageal cancer surgery.
- Thoracic surgical oncologist: A thoracic surgical oncologist is a surgeon who specializes in surgeries on tumors found inside the chest.
- Medical oncologist: A medical oncologist is a doctor who specializes in treating cancer with drugs, such as chemotherapy and targeted therapy.
- Radiation oncologist: A radiation oncologist is a doctor who specializes in treating cancer with radiation therapy.
You may want to find doctors who have a lot of experience with treating esophageal cancer.
Resources are available to help you find doctors who treat this disease:
- Your doctor may be able to refer you to specialists.
- You can ask a hospital, medical school, or medical society for names of specialists near you.
- NCI’s Cancer Information Service can give you information about treatment centers near you. Call 1-800-4-CANCER (1-800-422-6237). Or, chat using LiveHelp (https://livehelp.cancer.gov), NCI’s instant messaging service.
- Other sources can be found in the NCI fact sheet How To Find a Doctor or Treatment Facility If You Have Cancer.
Your health care team may also include an oncology nurse, a social worker, and a registered dietitian. If your airways are affected by the cancer, you may have a respiratory therapist as part of your team. If you have trouble swallowing, you may have a speech pathologist.
For help relieving or reducing pain, you may work with a specially trained doctor, a nurse, a palliative care team, or another pain control specialist.
Your health care team can describe your treatment options, the expected results of each option, and the possible side effects. Because cancer treatments often damage healthy cells and tissues, side effects are common. These side effects depend on many factors, including the type of treatment. Side effects may not be the same for everyone, and they may even change from one treatment session to the next.
Cancer of the esophagus is hard to control with current treatments. For that reason, many doctors encourage people with this disease to consider taking part in a research study (clinical trial) of new treatment methods. Research studies are an important option for people with any stage of esophageal cancer. See the Cancer Treatment Research section on page 30.
Questions you may want to ask your doctor about treatment options
- What are my treatment options? Which do you recommend for me? Why?
- What are the expected benefits of each kind of treatment?
- What are the risks and possible side effects of each treatment? How can side effects be managed?
- What can I do to prepare for treatment?
- Will I need to stay in the hospital? If so, for how long?
- What is the treatment likely to cost? Will my insurance cover it?
- How will treatment affect my normal activities?
- Would a treatment research study be right for me?
Second Opinion
Before starting treatment, you might want a second opinion about your diagnosis and your treatment options. You may even want to talk to several different doctors about all of the treatment options, their side effects, and the expected results.
Some people worry that the doctor will be offended if they ask for a second opinion. Usually the opposite is true. Most doctors welcome a second opinion. And many health insurance companies will pay for a second opinion if you or your doctor requests it. Some insurance companies actually require a second opinion.
If you get a second opinion, the second doctor may agree with your first doctor’s diagnosis and treatment recommendation. Or, the second doctor may suggest another approach. Either way, you have more information and perhaps a greater sense of control. You can feel more confident about the decisions you make, knowing that you’ve looked at all of your options.
It may take some time and effort to gather your medical records and see another doctor. In most cases, it’s not a problem to take several weeks to get a second opinion. The delay in starting treatment usually will not make treatment less effective. To make sure, you should discuss this delay with your doctor. Some people with cancer of the esophagus need treatment right away.
Surgery
Surgery may be an option for people with early-stage cancer of the esophagus. Usually, the surgeon removes the section of the esophagus with the cancer, a small amount of normal tissue around the cancer, and nearby lymph nodes. Sometimes, part or all of the stomach is also removed.
If only a very small part of the stomach is removed, the surgeon usually reshapes the remaining part of the stomach into a tube and joins the stomach tube to the remaining part of the esophagus in the neck or chest. Or, a piece of large intestine or small intestine may be used to connect the stomach to the remaining part of the esophagus.
If the entire stomach needs to be removed, the surgeon will use a piece of intestine to join the remaining part of the esophagus to the small intestine.
During surgery, the surgeon may place a feeding tube into your small intestine. This tube helps you get enough nutrition while you heal.
You may have pain from the surgery. However, your health care team will give you medicine to help control the pain. Before surgery, you may want to discuss the plan for pain relief with your health care team. After surgery, they can adjust the plan if you need more pain relief.
Your health care team will watch for pneumonia or other infections, breathing problems, bleeding, food leaking into the chest, or other problems that may require treatment.
The time it takes to heal after surgery is different for everyone. Your hospital stay may be a week or longer, and your recovery will continue after you leave the hospital.
See the Nutrition section for information about eating after surgery.
Esophageal cancer has spread to other parts of the body, such as the liver, lungs, or bones.
- Questions you may want to ask your doctor about surgery
- Do you suggest surgery for me? If so, what type?
- How will I feel after surgery?
- If I have pain, how can we control it?
- How long will I be in the hospital?
- Am I likely to have eating problems? Will I need a special diet?
- Will I need a feeding tube? If so, for how long? How do I take care of it?
- Who can help me if I have a problem?
- Will I have any lasting side effects?
- When can I get back to my normal activities?
Radiation Therapy
Radiation therapy is an option for people with any stage of esophageal cancer. The treatment affects cells only in the area being treated, such as the throat and chest area.
Radiation therapy may be given before, after, or instead of surgery. Chemotherapy is usually given along with radiation therapy.
Radiation therapy for esophageal cancer may be given to…
- Destroy the cancer
- Help shrink the tumor so that you can swallow more easily
- Help relieve pain from cancer that has spread to bone or other tissues
Doctors use two types of radiation therapy to treat esophageal cancer. Some people receive both types:
- Machine outside the body: The radiation comes from a large machine. This is called external radiation therapy. The machine aims radiation at your body to kill cancer cells. It doesn’t hurt. You’ll go to a hospital or clinic, and you’ll lie down on a treatment table. Each treatment session usually lasts less than 20 minutes. Treatments are usually given 5 days a week for several weeks.
- Radioactive material inside the body (brachytherapy): The doctor numbs your throat with an anesthetic spray and gives you medicine to help you relax. The doctor puts a tube into your esophagus. The radiation comes from the tube. After the tube is removed, no radioactivity is left in your body. Usually, one treatment session is needed. Because the treatment session lasts one to two days, you’ll probably stay in a special room at the hospital.
The side effects of radiation therapy depend mainly on the type of radiation therapy, how much radiation is given, and the part of your body that is treated.
External radiation therapy aimed at the chest may cause a sore throat, cough, or shortness of breath. You may feel a lump in your throat or burning in your chest or throat when you swallow. After several weeks of treatment, it may be painful to swallow. Your health care team can suggest ways to manage these problems. The problems usually go away when treatment ends.
External radiation therapy can harm the skin. It’s common for the skin in the chest area to become red and dry and to get darker. Sometimes the skin may feel tender or itchy. Check with your doctor before using lotion or cream on your chest. After treatment is over, the skin will heal.
You’re likely to become tired during external radiation therapy, especially in the later weeks of treatment. Although getting enough rest is important, most people say they feel better when they exercise every day. Try to go for a short walk, do gentle stretches, or do yoga.
Years after either type of radiation therapy, the esophagus may become narrow. If this happens, it may feel like food is getting stuck in your chest. Usually, a gastroenterologist can treat this problem.
The NCI booklet Radiation Therapy and You has helpful ideas for coping with radiation therapy side effects. Questions you may want to ask your doctor about radiation therapy
When will treatment start? When will it end? How often will I have treatments?
How will I feel during treatment? Will I be able to drive myself to and from treatment?
What can I do to take care of myself before, during, and after treatment?
How will we know the treatment is working?
What side effects should I expect? What should I tell you about?
Are there any lasting effects?
Chemotherapy
Most people with esophageal cancer get chemotherapy. It may be used alone or with radiation therapy.
Chemotherapy uses drugs to kill cancer cells. The drugs for cancer of the esophagus are usually given directly into a vein (intravenously) through a thin needle.
You’ll probably receive chemotherapy in a clinic or at the doctor’s office. People rarely need to stay in the hospital during treatment.
The side effects depend mainly on the drugs given and amount of chemotherapy that you get. Chemotherapy kills fast-growing cancer cells, but the drugs can also harm normal cells that divide rapidly:
- Blood cells: When drugs lower the levels of healthy blood cells, you’re more likely to get infections, bruise or bleed easily, and feel very weak and tired. Your health care team will check for low levels of blood cells. If your levels are low, your health care team may stop the chemotherapy for a while or reduce the dose of the drug. They may also give you medicines that help your body to make new blood cells.
- Cells in hair roots: Chemotherapy may cause hair loss. If you lose your hair, it will grow back after treatment, but the color and texture may be changed.
- Cells that line the digestive tract: Chemotherapy can cause a poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Your health care team can give you medicines and suggest other ways to help with these problems.
Other possible side effects include a skin rash, joint pain, tingling or numbness in your hands and feet, hearing problems, or swollen feet or legs.
When radiation therapy and chemotherapy are given at the same time, the side effects may be worse.
Your health care team can suggest ways to control many of these problems. Most go away when treatment ends.
The NCI booklet Chemotherapy and You has helpful ideas for coping with chemotherapy side effects.
Targeted Therapy
People with esophageal cancer that has spread may receive a type of treatment called targeted therapy. This treatment can block the growth and spread of esophageal cancer cells.
Targeted therapy for cancer of the esophagus is usually given intravenously. The treatment enters the bloodstream and can affect cancer cells all over the body.
During treatment, your health care team will watch you for side effects. You may get diarrhea, belly pain, heartburn, joint pain, tingling arms and legs, or heart problems. Most side effects usually go away after treatment ends.
You may want to rQuestions you may want to ask your doctor about chemotherapy or targeted therapy
- Which drug or drugs do you suggest for me? What will they do?
- What are the possible side effects? What can we do about them?
- When will treatment start? When will it end? How often will I have treatments?
- How will we know the treatment is working?
- Will there be lasting side effects?
ead the NCI fact sheet Targeted Cancer Therapies.
Nutrition
It’s important for you to be well nourished before, during, and after cancer treatment. Being well nourished may help you feel better, have more energy, and get the most benefit from your treatment.
However, esophageal cancer and its treatment can make it hard to be well nourished, and it may be hard for you to not lose weight. For many reasons, you may not feel like eating. For example, you may have nausea or trouble swallowing, and the foods you used to like to eat could now cause discomfort.
The NCI booklet Eating Hints has lists of foods to help with certain eating problems, such as trouble swallowing.
If you’re unable to eat, special treatments or other ways of getting nutrition may be needed. If the cancer in your esophagus makes it very hard to swallow food, your health care team may suggest that you have radiation therapy to shrink the tumor. Or, they may suggest that a plastic or metal mesh tube (stent) be put in your esophagus to keep it open. Another option is for you to receive nutrition through a feeding tube. Sometimes, intravenous nutrition is needed.
Nutrition After Surgery
If your stomach is removed during surgery for esophageal cancer, you may develop dumping syndrome. After meals, people with dumping syndrome may have cramps, nausea, bloating, diarrhea, and dizziness.
If you have dumping syndrome, a registered dietitian can help you learn how to be well nourished without making your symptoms worse. Here are some tips for preventing or controlling the symptoms of dumping syndrome:
- Try to eat at least 6 small meals each day.
- Sit up during meals and for at least 30 minutes afterward.
- Chew food very well.
- Eat mostly solid meals, and drink liquids between meals.
- Avoid very sweet foods and drinks.
- After surgery, ask your health care team whether you need a dietary supplement, such as calcium or vitamin B12.
Questions you may want to ask a dietitian about nutrition
- How do I keep from losing too much weight?
- How do I know whether I’m getting enough calories and protein?
- What are some sample meals that would meet my needs?
- How can I include my favorite foods without causing or worsening digestive problems?
Follow-Up Care
You’ll need regular checkups (such as every 3 to 6 months) after treatment for cancer of the esophagus. Checkups help ensure that any changes in your health are noted and treated if needed. If you have any health problems between checkups, contact your doctor.
Cancer of the esophagus may come back after treatment. Your doctor will check for the return of cancer. It may return in the chest or it may return in another part of the body, such as the liver.
Checkups also help detect health problems that can result from cancer treatment.
Checkups may include a physical exam, blood tests, chest x-rays, CT scans, endoscopy, or other tests.
NCI Highlights
- Report to the Nation Shows U.S. Cancer Death Rates Continue to Drop
- Education and Training for Health Professionals
- Cancer Trends Progress Report: 2011/2012 Update
Learning that you have cancer of the esophagus can change your life and the lives of those close to you. These changes can be hard to handle. It’s normal for you, your family, and your friends to need help coping with the feelings that a diagnosis of cancer can bring.
Concerns about treatments and managing side effects, hospital stays, and medical bills are common. You may also worry about caring for your family, keeping your job, or continuing daily activities.
Many people can help you manage these concerns:
- Doctors, nurses, and other members of your health care team can answer questions about treatment, working, or other activities.
- Social workers, counselors, or members of the clergy can be helpful if you want to talk about your feelings or concerns. Often, social workers can suggest resources for financial aid, transportation, home care, or emotional support.
- Support groups can also help. In these groups, people with esophageal cancer or their family members meet with other patients or their families to share what they have learned about coping with the disease and the effects of treatment. Groups may offer support in person, over the telephone, or on the Internet. You may want to talk with a member of your health care team about finding a support group.
- NCI’s Cancer Information Service can help you locate programs, services, and NCI publications. Call 1-800-4-CANCER (1-800-422-6237). Or, chat using LiveHelp (https://livehelp.cancer.gov), NCI’s instant messaging service.
For more information on this and other symptoms or diseases, contact our offices at 210-268-0124 for an appointment.

